Atopic eczema
Atopic eczema, also known as atopic dermatitis, is a common chronic inflammatory skin condition occurring at any age. How to recognize atopic eczema and how to treat it when it appears?
What are the symptoms of atopic eczema?
- Dry skin
- Itching
- Inflammation of the skin (mostly with bursting blisters)
How to recognize atopic eczema?
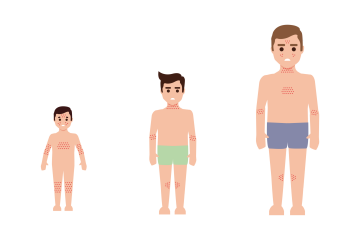
The symptoms vary with age.
In patients with severe eczema, the skin may result in so-called lichenification, which refers to hard and rough patches. The child's mental health can be affected due to visible symptoms, making them uncomfortable and anxious. Ceaseless itching challenges the patient’s everyday life.
What do asthma and eczema have in common?
Eczema, asthma and allergic rhinitis are atopic diseases. Atopy has a hereditary component. Atopic disease development starts with eczema in early childhood, continues with allergic rhinitis and later with asthma. We call it the atopic march, but not all conditions always occur.
Other trigger factors can make eczema worse:
- Contact and inhaled allergens – dust, pollen, dust mites, animals, fur, molds
- Ingested allergens – milk, eggs, fish, seafood, citruses, kiwi, pineapple, mango, strawberries, currants, tomatoes, sweet peppers, celery, parsley, horseradish, chocolate, cocoa, poppy seeds, honey, nuts, legumes, soy, mustard, grains, cabbage, canned foods, certain spices, smoked meats
- Contact with irritants – how water, soaps, detergents, chlorine, cigarette smoke, sand, polyester, wool, leather
- Microorganisms – bacteria, viruses, molds and yeast
- Emotional distress
- Hormonal imbalance – growing up, during pregnancy, birth, menopause, PMS
- Cold and hot environments
What’s the treatment for atopic eczema?
Treating eczema is a long-term process requiring close cooperation between the doctor and the patient (even their family members). Allergists and dermatologists participate in the treatment, and immunologists or psychologists are often welcome.
Eczema is treated with topical (local) and systemic (pills, intravenously) medication.
FAQs
What are the risk factors for atopic eczema?
- Genetics – Many people with a family history of eczema are affected. The presence of eczema in the family history increases the risk of developing it 3× more.
- Skin barrier defect – Due to this condition, excessive water loss through the skin causes it to dry. The skin is more sensitive to trigger factors such as allergens and other substances, making eczema worse.
- Immune response – The immune system protects the body against harmful stimuli. Eczema patients have a more robust immune response towards even unharmful stimuli.
- Environmental factors – According to the so-called hygiene hypothesis, excessively clean environments in early childhood take part in eczema development. While “children in the countryside” are usually more exposed to harmful substances improving their immune system, the “children in the city” tend to live in a cleaner environment, making them react to unharmful stimuli as well.
- Infection – Friendly bacteria inhabit and protect our skin. Disrupting this microbiome leads to low diversity and atopic eczema development.
What’s the diagnosis process?
A dermatologist can diagnose you with atopic eczema depending on the course of the condition and symptoms. A blood test, skin sample, or eventually allergy testing, can contribute to the diagnosis. If you suspect you have eczema, see your general practitioner, who’ll send you to a dermatologist for examination.
Is it possible to prevent atopic eczema?
There are no preventative measures in the true sense of the word. But, you can prevent eczema from getting worse by avoiding the triggers and adherence to treatment.
How?
- Healthy diet (rich in antioxidants) – avoid foods triggering the allergy.
- Do not smoke (not even e-cigarettes).
- Maintain adequate room temperature to avoid sweating.
- Wear eczema-friendly clothing – avoid tight, wool or leather clothing; choose rather airy cotton pieces.
- Limit contact with animals and triggering substances – such as softeners, detergents, and chlorine.
- Adjust your home – humidify the air, make it dust-free and colder, no carpets and curtains, hoover and ventilate regularly.
- Take care of your skin – use appropriate soap, shampoo and cosmetics, and avoid long hot baths.
- Avoid scratching; therefore, infections – moisturize the skin and trim your fingernails short.
- Manage the stress – you can’t avoid the stress completely these days, but you can manage it with regular exercise, meditation or breathing exercises.
Donate to Loono
Your donation helps us to buy new models, print leaflets and pay our lecturers and administrative workers for their work.
Donate to Loono
Your donation helps us to buy new models, print leaflets and pay our lecturers and administrative workers for their work.